Tips from the Experts: How to Reduce the Risk of Infection in Healthcare Facilities
Modified from Donskey CJ. Am J Infect Control 2023
The theme for World AMR Awareness Day is AMR is invisible, I am not.
Kim Neudorf PFPSC:
AMR (antimicrobial resistance) is a complicated term. To simplify, some refer to AMR as superbugs. Patients may not pay much attention to AMR until their infection does not respond to medication treatment, such as an antibiotic prescription. When these medications are ineffective, the infection lingers, hospitalizations are prolonged, and there is a possibility of death. We all understand infection. Yet, being infected with one of these stubborn organisms is worrisome for the patient, family, and the healthcare team.
In past campaigns, Patients for Patient Safety Canada (PFPSC) has focused on educating the public about the proper use of medications, such as antibiotics. Messages such as, “antibiotics will not cure a virus”, or “not every condition of a cough, fever or runny nose requires a prescription,” are important because the overuse and misuse of antibiotics contributes to the growing problem of AMR.
Infection acquired while receiving health care is a patient safety concern. PFPSC represents the patient voice that includes experiences of disfigurement, stigma, fear, suffering, disability and possible death originating with an AMR organism. This year PFPSC draws attention to prevention of infection. Actions such as keeping cuts and abrasions clean and covered, frequent hand hygiene, and vaccinations can reduce infections and reduce the need for an antibiotic. We also remind the public about the importance of cleaning and disinfection (C&D) within healthcare facilities and the role patients have. Yes, these microorganisms are invisible, but C&D and active measures to prevent infection should not be. Preventing infections in healthcare facilities reduces the overuse of antibiotics, which contributes to AMR.
PFPSC turned to the experts, Jim Gauthier and Curtis Donskey for information about the importance of the C&D process in healthcare facilities and how patients can protect themselves.
Jim Gauthier MLT CIC:
Cleaning and disinfection (C&D) within healthcare facilities is conducted at least once per day, but care occurs all day, every day. Microorganisms like viruses, bacteria and fungi thrive in dirty healthcare environments.
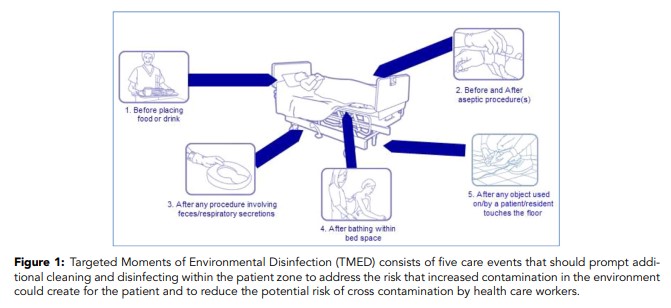
‘Your Four Moments for Hand Hygiene’ informed healthcare providers of when to clean (sanitize) their hands, depending on the care provided. Do we need the same reminder for the healthcare environment and standard care practices? Should an overbed table be cleaned and disinfected before a meal tray is placed? If healthcare staff are caring for a wound, central line, IV, or other device, should some C&D occur before and after that procedure? Feces and saliva contain millions of bacteria, and some C&D is probably required while caring for a patient (changing a brief, suctioning) within their bedspace. Many patients are not able to get out of bed, and are bathed within their bedspace, which could leave microorganisms on surfaces near the patient. The floor can never be kept free from microorganisms, and anything that touches the floor (cell phone, charger, call bell, etc.) must receive C&D before being given back to the patient…there is no ‘5 second’ rule in a hospital!
These are targeted moments of environmental disinfection and were published as a commentary in 2020 (Gauthier, 2020). A concept of “If, during care, you touched it or used it: Disinfect it” can keep superbug numbers to a minimum, and also keep all harmful microorganisms in very low numbers around our patients.
Curtis Donskey MD:
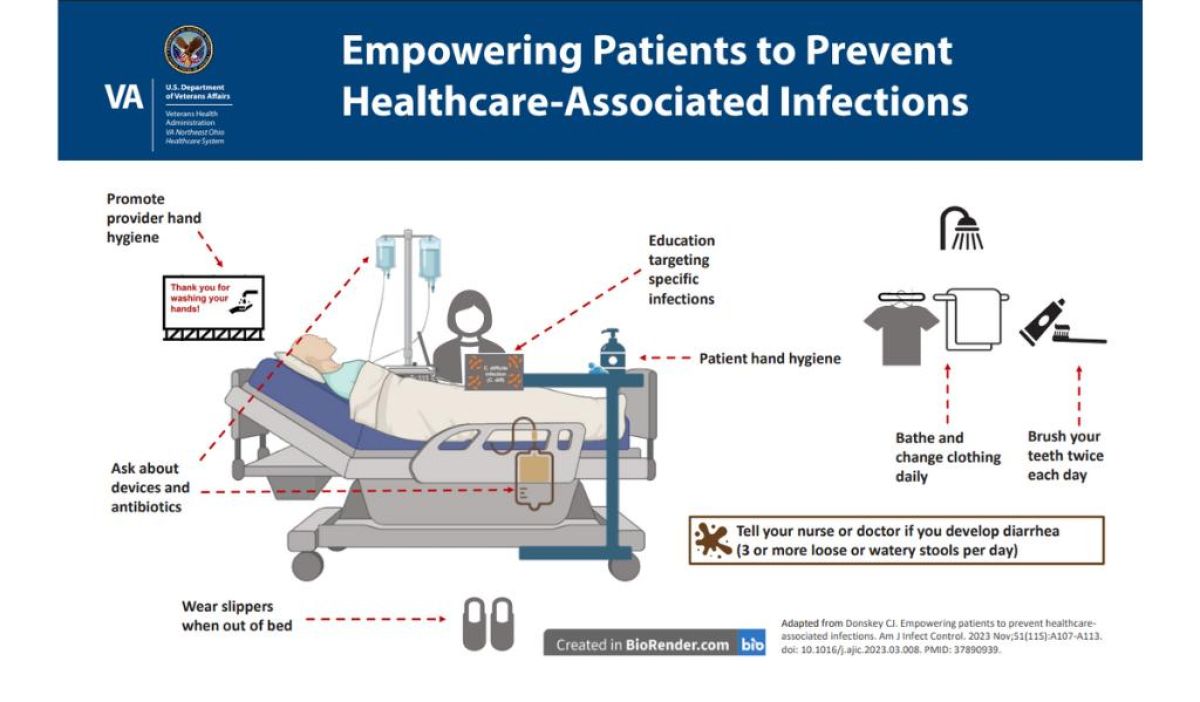
In recent years, there has been increasing interest in empowering patients to serve as partners in efforts to prevent healthcare-associated infections. In addition to C&D, there are several simple measures that patients can take to reduce their risk of acquiring an infection. An evidence-based bundle illustrating several of these measures is shown in the infographic (modified from Donskey CJ, 2023). These measures include:
- Remind providers to perform hand hygiene. For patients too shy to discuss hand hygiene with providers, posters displaying the message “Thank you for washing your hands!” can be effective in reinforcing hand hygiene.
- Ask providers about devices and antibiotics. Devices and antibiotics can have adverse effects and should be discontinued as soon as they are not needed.
- Perform personal hand hygiene frequently. Hand hygiene will eliminate any microorganisms acquired from contaminated surfaces.
- Bathe and change clothing daily. Bathing and changing clothing is important for patients because clothing and skin can become contaminated with bacteria.
- Brush teeth twice each day. Bacteria that build up on teeth can cause pneumonia if they are aspirated into the lungs. Brushing teeth twice each day can reduce the risk for pneumonia.
- Wear slippers when out of bed. Bacteria on the floor can be acquired on socks and then transferred to hands and other surfaces. Wearing slippers can reduce the risk for transfer of bacteria from the floor if they are removed before putting feet in or on the bed.
- Education targeting specific infections. Patients should ask for educational materials so they understand measures they can take to reduce the risks for themselves and their family members.
- Tell your nurse or doctor if you develop diarrhea (3 or more loose or watery stools per day). Let your providers know if you develop diarrhea because antibiotics and some other medications are common causes of diarrhea.
The authors
Jim Gauthier is a medical technologist. Jim worked in general microbiology, water and food bacteriology, and parasitology. While in the lab, Jim found his love of infection prevention and became board-certified in 1990. Jim has worked in, or consulted to acute care, long term care, medical and dental clinics, optometrists, schools, industry, public health and even funeral homes. Jim has lectured throughout North America and internationally in England, Germany, France, Portugal, Hong Kong and New Zealand.
Curtis Donskey MD is an Infectious Diseases physician and hospital epidemiologist at the Louis Stokes Cleveland VA Medical Center and a Professor of Medicine at Case Western Reserve University. His research focuses on development of improved strategies to prevent infections due to healthcare-associated pathogens.
Kim Neudorf is a member of Patients for Patient Safety Canada. She advocates for infection prevention and control, AMR awareness, Sepsis awareness, Frailty Prevention and management, and Alzheimer’s prevention and management. She paints with watercolours and ink.
References:
Gauthier J, Teska P, Calabrese C. Targeted moments of environmental disinfection. Jt Comm J Qual Pat Safety 2020;46(3):167-72.
Adapted by Donskey CJ, Empowering patients to prevent healthcare-associated infections. Am J Infect Control 2023;51(11S):A107-A113.